Why I Had a Mastectomy at 21
mas·tec·to·my [ /maˈstektəmē/ ] noun. Surgery.
1. a surgical operation to remove a breast.
I was 21 years old when I had a prophylactic bilateral mastectomy. I had just graduated from college a week before the operation, and no, I didn’t have breast cancer. So why the hell would I do this? Let me tell you the story, starting from the very beginning this time.
Losing Mom
I was five years old when my mom was diagnosed with breast cancer.
At that age, I didn’t really understand what that meant. I knew my mom was sick a lot, and some days she didn’t want to get out of bed. I knew I felt like I was helping if I could rub her back while she got sick in the toilet each night. I knew my mom didn’t have hair like the other moms, and sometimes the other kids would ask why.
I was 9 when my mom told me she was going to die. She was gone a year later.
I was at 5th-grade camp when she "left." That's what I called it then.
My teacher pulled me out of camp and drove me home. I remember being angry that he wouldn't tell me what was happening. Being mad I had to leave camp. Secretly knowing what was likely the reason for my departure. Feeling guilty that I was angry at all. It was a lot to process at age 10.
When we arrived at the house, my little brother was standing out front alone. “She’s gone.”
The days that followed were filled with visitations, funerals, casseroles. I remember concern from others that I wasn’t crying enough. I did cry, for the record. But I did it alone.
What people didn’t understand was that my mom had been gone for quite some time. We mourned her the day she told us she was stopping care, and we had watched her suffer through treatments for years before and after that day.
The point of sharing this information isn't to get you to pity me. I share it so that, hopefully, you can understand why I grew up scared as hell of ever going through the same thing.
For my family, breast cancer wasn't something we did a charity walk to raise money for once a year. It was real, it was hell, and I was terrified of it.
What's My Risk?
Let’s fast forward six years. I'm now 16 and making my first visit to the OB/GYN. This is the first time I have had to consider the risk of hereditary breast cancer. Let’s look at the risk factors:
Family History: My doctor explained that both my mom’s sister and aunt had had breast cancer. When multiple relatives are affected, it raises suspicion of a genetic mutation.
Age of Diagnosis: My mom was diagnosed at just 34 and was already close to stage IV when she found it. BRCA mutation carriers also tend to be diagnosed younger.
Presence of a Mutation: We later discovered my aunt had tested positive for the BRCA2 mutation. If my mom had it too, I had a 50% chance of inheriting it.
“You need to see a genetic counselor and get on top of this.” So I went.
I spent hours with two counselors and my family, mapping out our entire medical history. They recommended genetic testing.
I decided then—if I had the mutation, I’d take preventative action.
Finding Out I’m a Mutant
Two years later and a freshman in college, I was 18 and finally able to get tested. Just a quick blood draw and the sample was off to the lab.
There was a 50/50 chance I carried the BRCA2 mutation. If I did, I’d become what they call a "high-risk patient." Here's what that means:
Increase in breast cancer risk: My lifetime risk would go up from the average of 13% to up to 69%. For BRCA1 mutation carriers, the risk goes up to 72%.
Increase in ovarian cancer risk: My lifetime would go up from the average of 1.1% up to 29%. For BRCA1 mutation carriers, the risk goes up to 58%.
Earlier age of diagnosis: High-risk patients are often diagnosed at much younger ages. My mom was only 34 when she was diagnosed and her cancer was metastatic, meaning it had spread to other parts of her body, and her chance of survival was low.
Insurance covered most of the test, and since my aunt had tested positive previously, the cost was even more affordable. We paid about $400 out-of-pocket in 2011—far less than the ~$3,500 it would’ve cost without a known family mutation. That said, accessibility to testing has made it more affordable today.
Six weeks after my blood sample was taken, during my first quarter of college, I stepped out of stats class and got the call.
“You’re BRCA2 positive.” Awesome.
Note: For medical decisions, always go through a certified testing lab—home kits aren’t a substitute for clinical guidance.
Options for Prevention
I started seeing a high-risk doctor to assess my options for prevention shortly after getting my results. He told me I had a few choices:
Option 1:
Increased Screenings
Get regular breast screenings with a focus on early detection, but overall take no preventative action.
Why option 1 didn’t work for me:
Catching cancer early results in much higher survival rates. However, once you have cancer once you’re up to 10x more likely to get it again. I’d rather avoid that risk altogether.
Option 2:
Preventative Chemotherapy
Take low dosages of chemotherapy to reduce risk
Why option 2 didn’t work for me:
While low dosages of chemo can be effective in prevention, I was terrified of putting my body through even an inkling of what I saw my mom go through during chemotherapy.
Option 3:
Preventative Surgery
Undergo a prophylactic bilateral mastectomy. In laymens terms: remove all my breast.
Why Option 3 did work for me:
This option reduced my lifetime risk by 95%, putting my personal risk lower than the general population. It’s permanent.
Important: This was my decision. It won’t be the right one for everyone. Talk to your doctors. Read up on your choices. Think about what kind of life you want. Then decide. You’ll figure it out—I promise.
I had to stand up for my choice. My surgeon pushed for just increased screenings saying: “Most women just want to get through their 20s first. They don’t want to worry about their appearance changing.”
But being high-risk, I wasn’t just thinking about my 20s—I was thinking about my 30s, 40s, and beyond. About not getting sick at all. To me, appearance was the least of my concerns.
My mom was diagnosed young, and I knew how easy it’d be to keep pushing the surgery off. After some back-and-forth and reassurance that this wasn’t a spur-of-the-moment decision but something I’d been thinking about most of my life, my doctor agreed.
We scheduled surgery for May 11, 2015, the week after I graduated from college.
Prophylactic Bilateral Mastectomy
Let's break this operation down a little:
Prophylactic = preventative
Bilateral = both sides, meaning both breasts in this instance
Mastectomy = a surgical operation to remove a breast
The morning of the procedure I only cried once.
The operation was four hours long, and I stayed one night in the hospital. I was on so many drugs I didn’t know what was going on, what time of day it was, or who was in the room. I didn’t feel any pain until the morning.
When I woke up, the pain was different than I expected. Most of my nerves were damaged during the operation, so I couldn’t actually feel the 8-inch purple incisions across each side of my chest. The cuts looked worse than they felt. All I felt was immense soreness.
The first time I took my bandages off was jarring, to say the least. You can do the research. You can know what things are going to look like. But seeing myself for the first time post-op was not an easy experience.
Where my chest had once been now sat two deflated surgical expanders, each slashed with gruesome-looking incisions. I had 2 surgical drains coming out of each of my sides, four in total.
The good news? The initial recovery was fairly quick. I was off painkillers and muscle relaxers within a week.
Honestly, I think boredom sped things up. I binged so many episodes of My 600 Pound Life. And my doctor said I could drive once I was off the pain meds, so I got off the pain meds.
The worst part? The JP drains. I had two on each side of my ribs to prevent fluid buildup. They were gross, hard to hide, and constantly got caught on doorknobs. Since they were open wounds, I couldn’t shower normally until they were out. I hated those things so much.
Breast Reconstruction
Breast reconstruction is the process of plastic surgery to rebuild breasts after a mastectomy. For some, it’s a big part of the emotional healing journey while others choose to stay flat.
Six weeks after my mastectomy, I started reconstruction. During my initial mastectomy, I had temporary implants—called expanders—placed under my pectoral muscles. This is called under-the-muscle (UTM) reconstruction.
The expanders were rock hard and not very natural-looking. Every, a nurse injected fluid through a port to slowly “inflate” them. It sounds painful, but thanks to nerve damage I barely felt it. I mostly had some muscle soreness after. Since the process took several months, I stuffed my bra to make my clothes fit in the meantime.
Once we reached the right size, I waited for things to settle before the last surgery to swap in my permanent implants. The exchange surgery was much easier, with about 1–2 weeks of recovery. These were also placed under the muscle.
The full expansion process took about six months. I couldn’t return to my original size because the skin had thinned from stretching. This is worth discussing with your doctor if you’re a bustier person going through this process and hoping to return to your original size.
Both surgeries totaled around $90,000, but insurance covered most of it. I paid about $5K out-of-pocket over a few years and finally finished paying it off in 2021.
Breast Reconstruction Pt. 2
In July 2021, I revisited my reconstruction to move the implants out from underneath the pectoral muscles. The goal was to achieve more comfortable results without stretching my pec muscles over the implants which never felt comfortable with my active lifestyle. I always felt like I was being held in, wrapped in something tight. I'm not sure how else to explain it.
I found out when I woke up from the surgery that both of my implants were ruptured so it was lucky I chose to move forward with the revision.
My surgeon repaired my pectoral muscles by sewing them back down, placed new implants above the muscle, and used a process called fat grafting to improve the final appearance and allow for a smaller implant to be used.
Fat grafting is the process of harvesting fat cells from other parts of the body and injecting them into the chest. I had to go back after the first procedure for one additional fat grafting session since the body absorbs about 30% of the fat cells that are transferred.
I'm really happy with the results and am so glad I took the plunge to improve my comfort.
Insurance covered the cost of the revisions so I only had to pay my insurance plan's annual deductible. Under The Women's Health and Cancer Rights Act insurance companies should cover all reconstruction and revisions for mastectomy patients. My surgeon was out-of-network but was kind enough to not balance bill me the 20% of the cost that my insurance wouldn't cover after the deductible.
I haven't gone forward with nipple reconstruction because I haven't seen much work in that field that looks realistic enough to justify going back to wearing bras regularly. So yeah, you read that right, I don’t have nipples. I did find one tattoo artist in Ireland who does AMAZING restorative tattoo work who I may schedule with one day.
Physical and Emotional Healing
Total recovery, both physical and emotional, was slow. It was frustrating. I couldn’t lift my arms or sleep on my stomach for months. I went through numerous months of reconstruction over 7 years. The second round of reconstruction was painful and long and had complications.
It took years to regain my upper body strength. Years to wear a top that showed my scars without thinking twice about it. Years to regain confidence in my physical appearance. But I got through it all and I haven't looked back since.
Since my mastectomy, I’ve felt like a giant weight has been lifted knowing my risk is lowered. While my risk is now lower than the general population, there's still risk. So I do my monthly self-exams too.
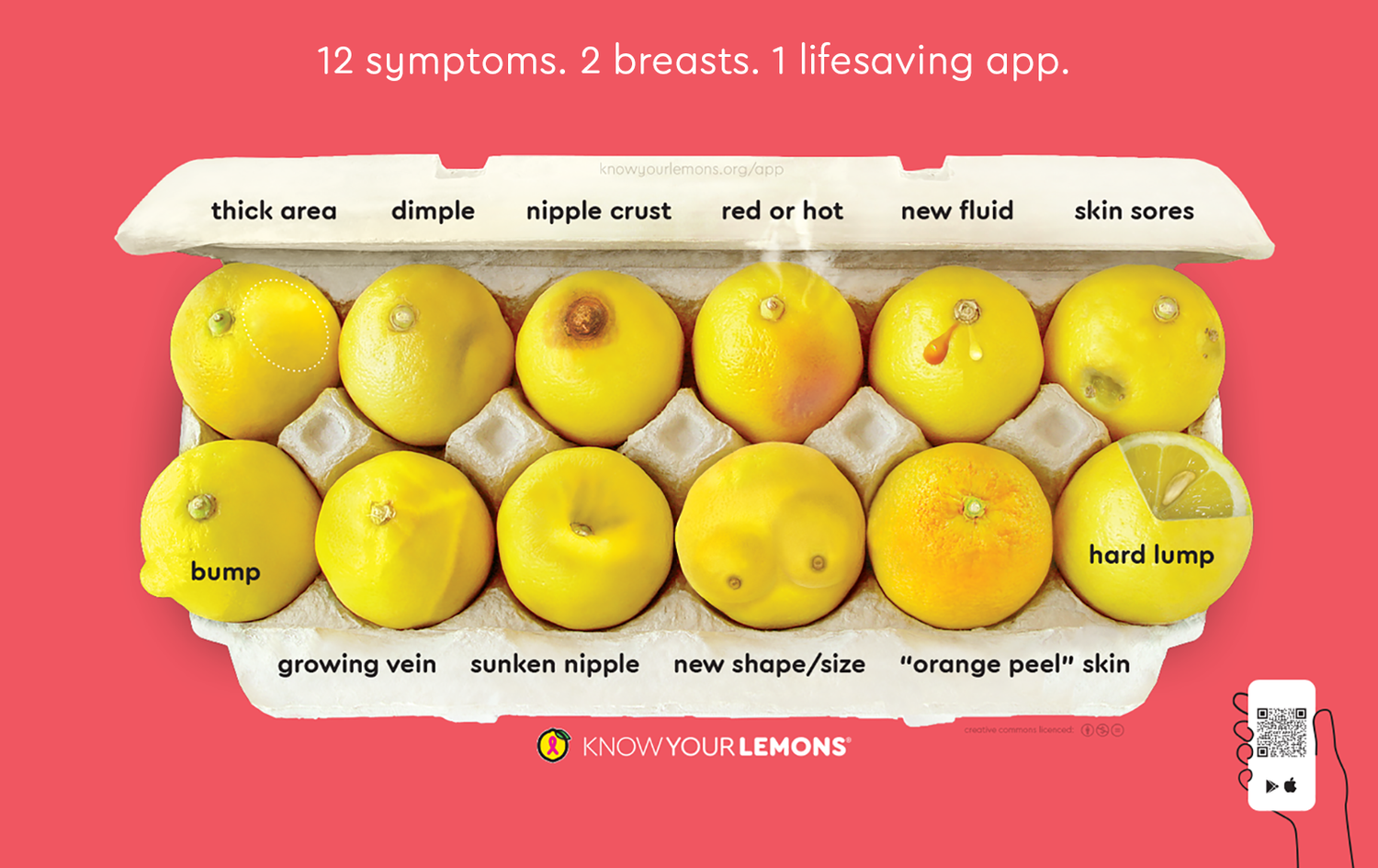
I've also found a lot of joy and healing in teaching others about breast cancer risk by becoming an educator with Know Your Lemons, a global nonprofit with a mission to save lives by reducing late-stage breast cancer diagnoses through education.
What's Next: Ovarian Cancer Risk
The other half of the BRCA mutation is that you also have an increased lifetime risk of ovarian cancer.
For now, I get yearly ultrasounds to check my ovaries and make sure they're healthy. If my doctor sees something concerning, I get a CA125 cancer antigen blood test and go back every six weeks for follow-up ultrasounds until the spot goes away. So far, it's only been cysts. Unfortunately, insurance only covers one of these ultrasounds a year, so any follow-ups I have to get usually cost me $300 out of pocket each time. Gotta love American healthcare.
Starting next year at age 30 I'll double up and get an ultrasound and a CA125 blood test every six months.
By age 45 I'll have my ovaries and fallopian tubes removed. This procedure is called a prophylactic bilateral salpingo-oophorectomy— what a mouthful. It took me a few years but I think I'm finally able to pronounce it correctly.
This procedure is recommended by age 35 for BRACA1 carriers and by 45 for BRCA2 carriers. While I still have some time before I reach the cap on the recommended age, I'm also growing increasingly tired of the anxiety and fear that come with my annual scans as I get older. So I'll probably get ahead of that in a few years.
Curious About Your Own Health?
Early detection saves lives. Here are some numbers:
Only ~5-10% of breast cancer cases are tied to genetic mutations. That means more than 90% of breast cancer cases are not tied to family history. Prioritize monthly self-exams and annual mammograms regardless of your family history.
You could have a 99% survival rate if you catch your cancer before it spreads. The longer cancer exists in your body the worse your chances of survival get. Check out the data below:
How to be proactive with your health:
Complete a monthly self-exam. Don't know how? Check out this guide from KnowYourLemons.org for direction! They also have an awesome app that will send you reminders and walk you through the self-exam process.
Schedule a yearly mammogram once you hit age 40, or 10 years prior to the age of a diagnosed family member if you have a family history. If cost is a hurdle, here's a resource to find free mammograms.
Have discussions about your family history of cancer to identify risk factors.
Host a breast health class by reaching out to me! I'm certified with Know Your Lemons and teach in-person (local to ATX) and virtual classes year-round.
What if I have a family history?
If you're worried you may be at a higher risk based on your family history:
1. Have a conversation about the history of cancer with your family
2. Do some research. Here are a few resources to get you started:
Risk Factors: This resource shares factors that could increase your risk.
Risk Assessment: This KnowYourLemons app has a risk assessment quiz that helps determine your risk level and provides you with a custom screening plan.
Screw You Cancer: Caitlin Brodnick shares her life-changing decision to have a preventative double mastectomy after learning she’s BRCA1-positive. This video series was really helpful for me as I figured out what I was getting myself into.
3. Talk to your doctor and a genetic counselor
4. Consider genetic testing
Make a decision that is right for YOU about how you can best be proactive with your health.
I’m not a professional, but I’m happy to share my experience. Questions, comments, concerns? Reach out any time. You can also follow me on Instagram or TikTok for monthly self-exam reminders.
X
Amanda Hagley
hagleyamanda@gmail.com